STANDARD: Prescribing Benzodiazepines and Z-Drugs
PREAMBLE
This Standard establishes the standard of practice and ethical requirements of all registrants in relation to prescribing benzodiazepines and/or z-drugs (zopiclone, eszopiclone, zolpidem) for maximum safety for all patients whether in the community or in a health care facility. This Standard does not apply to the use of these drugs in the treatment of cancer, palliative and end-of-life patients, seizure disorders, bipolar/psychotic disorder, and acute alcohol withdrawal. It is strongly recommended that the clinical indication and, if the prescribing is off label, a statement to that effect, be included.
Medical evidence of the risk to benefit ratio of prescribing benzodiazepines and/or z-drugs has been altered over time, so prescribing these drugs must be in accordance with current medical knowledge. This Standard recognizes that in prescribing benzodiazepines and/or z-drugs each registrant exercises their clinical judgment, which is to be that of a registrant acting reasonably in the circumstances with current medical knowledge.
POLICY
1. GENERAL
1.1 Reasonable efforts are to be used to optimize non-pharmacological treatment modalities first (i.e., Cognitive Behaviour Therapy, improved sleep habits, elimination of caffeine, etc.) if available, and then optimize non-benzodiazepines or non-z-drug treatment modalities
1.2 To mitigate risk of harm the registrant must review the patient’s current and past medications utilizing PIP and/or the eHR Viewer, or consult with a pharmacist. This will mitigate the risk of harmful drug interactions and combinations and will alert physicians to prescriptions from multiple providers.
1.3 Registrants must prescribe the lowest effective dosage of benzodiazepines or z-drugs for the shortest possible duration and only exceed the maximum recommended dosage in exceptional circumstances and document the rationale appropriately.
1.4 Long-term use must be supported by current clinical evidence.
1.5 Discuss the following with the patient and document it in the medical record:
- 1.5.1. Treatment goals including specific and realistic goals and an eventual possible discontinuation strategy;
- 1.5.2. Non-pharmacological therapies;
- 1.5.3. The benefit/risk of long-term benzodiazepines and z-drugs;
- 1.5.4. Overall risks associated with treatment; and
- 1.5.5. The impairment caused by these drugs (driving, operating heavy machinery, or performing safety sensitive tasks, providing child or elder care).
1.6 Registrants must carefully consider all concurrent medical conditions in the context of decisions to prescribe or continue to prescribe these medications:
- 1.6.1. Heart failure, obesity, sleep apnea, chronic lung disease, alcohol and substance use disorders and renal or hepatic insufficiency and other chronic conditions compound the risk of these medications in unique ways.
- 1.6.2. Current or planned pregnancy.
- 1.6.3. Patients must be regularly screened for the presence or emergence of mental health disorders (particularly mood and substance use disorders) which may complicate management.
- 1.6.4. In the course of managing patient care on these drugs (particularly while tapering), a substance use disorder may develop or reveal itself, and physicians must be able to appropriately diagnose and manage the patient’s care needs.
1.7. In the course of managing patient care on these drugs (particularly while tapering), a substance use disorder may develop or reveal itself, and physicians must be able to appropriately diagnose and manage the patient’s care needs.
- 1.7.1. Appropriate care management can include referral to a physician with expertise, if available, and can include slow tapering of benzodiazepines and z-drugs to minimize the effects of withdrawal. Periodically attempt a trial of slow tapering (and if possible, collaborate with a trusted pharmacist identified by the patient).
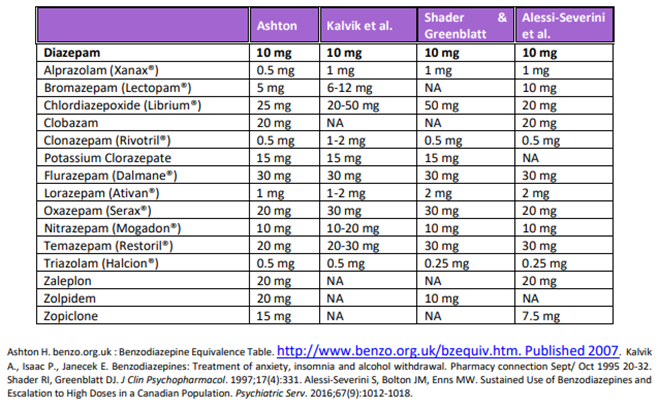
- 1.7.2. Use tapering guidelines and equivalency tables referred to in the Contextual Information attached to this Standard of Practice.
- 1.7.3. Appropriate care management does not include abruptly discontinuing or an ultra-rapid decrease of these drugs after long term use.
- 1.7.4. Where tapering is not feasible, if there is documented benefit to the patient outweighing the potential harms, then continue with the treatment. Tapering of long-term benzodiazepines and/or z-drugs is difficult, though possible.
1.8 Combining benzodiazepines and/or z-drugs or with other medications compounds risk of harm:
- 1.8.1. If prescribing benzodiazepines and/or z-drugs, physicians must consider potential drug interactions with prescribed, over the counter, and recreational psychoactive substances including alcohol, opioids, gabapentin, and other benzodiazepines, dimenhydrinate and diphenhydramine, and document their advice to patients;
- 1.8.2. If patients with complex care needs are receiving multiple sedating medications, the physician must consider seeking the opinion of relevant consultants such as psychiatrists, pain specialists/experts, addiction medicine specialists/experts, pharmacists, and others to work toward a collaborative medication regimen that minimizes risk as much as possible.
- 1.8.3. Only in exceptional circumstances prescribe opioids together with benzodiazepines and/or z-drugs. Patients must be informed of the increased risks (including death) with this combination, and the discussion must be thoroughly documented.
- 1.8.4. Only in exceptional circumstances prescribe two or more benzodiazepines and/or z-drugs concurrently unless in the context of a taper.
1.9. Registrants must be aware of and comply with statutory reporting duties to any relevant authorities (e.g. Transport Canada, SGI, etc.) if the patient’s disease or disability, or a treatment prescribed, is expected to cause impairment.
2. ELDERLY PATIENTS
2.1 For older adult patients, recognize that new starts of benzodiazepines and z-drugs must be carried out with extreme caution and not be used as first choice for insomnia, agitation, or delirium, nor for managing behaviours arising from dementia and delirium.
2.2 Ensure that dosing takes into consideration declining renal, hepatic and cognitive function and polypharmacy in older adult patients.
2.3 In prescribing for older adult patients, the registrant must recognize and discuss with the patient additional risks, including but not limited to:
- 2.3.1. Falls and subsequent fractures related to sedation, confusion, drowsiness and postural instability;
- 2.3.2. Impairment of psychomotor skills, judgment, and coordination increases the risk of motor vehicle and other accidents;
- 2.3.3. Negative effects on cognition, memory, delirium and a possible link to cognitive decline and dementia.
Contextual Information & Resources
The Contextual Information and Resources are provided to support registrants in implementing this Standard of Practice. The Contextual Information and Resources do not define this Standard of Practice, nor should it be interpreted as legal advice. It is not compulsory, unlike a Standard of Practice. The Contextual Information and Resources are dynamic and may be edited or updated for clarity, new developments, or new resources at any time.
Background
Medical evidence of the risk to benefit ratio of prescribing benzodiazepines and/or z-drugs has changed over time, so prescribing these drugs must be in accordance with current medical knowledge. Drugs of dependence have important therapeutic uses, but there is a need to ensure the prescribing of these medicines is clinically appropriate. In the past two decades clinical guidelines have recommended against long-term use of benzodiazepines and z-drugs. The conditions where benzodiazepines are most commonly prescribed (anxiety and insomnia) remain sources of debate in medical circles. Physicians must consider multiple factors when prescribing benzodiazepines. Good clinical judgment and an evidence-informed approach remain key to safe and appropriate prescribing. The Standard tries to strike the best balance between the benefits of benzodiazepines and z-drugs in contrast to the risks.
General Risks of Benzodiazepines and/or Z-Drugs
Benzodiazepines and Z-Drugs carry significant risk such as:
- Sedation, confusion, drowsiness and postural instability contributing to the risk of falls and subsequent fractures;
- Impairment of psychomotor skills, judgment, and coordination increasing the risk of motor vehicle accidents;
- Negative effects on cognition and memory, delirium, drug-related pseudo dementia and a possible link to cognitive decline and Alzheimer’s disease;
- Dependency and misuse potential;
- Risky interaction with medications or herbals;
- Sleep automatism (in the case of z-drugs), including food binging, and even driving while asleep or in a sleep-like state.
The Standard recognizes that:
- Initiating benzodiazepines and/or z-drugs in hospital substantially increases the risk of long-term use and dependency.
- Cognitive behavioural therapy, brief behavioural interventions and tapering protocols have a proven benefit in sedative-hypnotic discontinuation and are also beneficial in improving sleep.
- 13 people would have to be treated with a benzodiazepine and/or z-drug for 1 person to experience improved sleep. Alternatively, only 6 people would have to be treated with a benzodiazepine and/or z-drug for 1 extra person to experience an adverse outcome. [BMJ: doi: 10.1136/bmj.38623.768588.47(published 11 November 2005)
Risks of Prescribing Benzodiazepines and/or Z-Drugs to Elderly Patients
Benzodiazepines and/or z-drugs have been identified as problematic medications for use in older adults and carry significant risks. Large scale studies consistently show that the risk of motor vehicle accidents, falls and hip fractures, leading to hospitalization and death, can more than double in older adults taking benzodiazepines and/or z-drugs. Older patients, their caregivers and their health care providers should recognize these potential harms when considering treatment strategies for insomnia, agitation or delirium.
Benzodiazepines and Z-Drugs carry significant risks beyond those for the general patient population:
- Sedation, confusion, drowsiness and postural instability contributing to the risk of falls and subsequent fractures;
- Further impairment of psychomotor skills, judgment, and coordination increasing the risk of motor vehicle accidents
- Negative effects on cognition and memory, delirium, drug-related pseudo dementia and a possible link to cognitive decline and Alzheimer’s disease.
Benzodiazepine Receptor Agonist Equivalency Estimates
(Diazepam 10mg as reference)
Deprescribing
Gradual dose reduction and supervised tapering is the central tenet and preferred strategy in discontinuing benzodiazepine and z-drugs.
Working with a Pharmacist
Per the CMPA, pharmacists have professional, ethical and legal responsibilities for implementing therapeutic plans. Physicians and pharmacists are independent providers and each owes a separate duty for the care that falls within their individual scope of practice. There is a need for efficient and effective communication between physicians and pharmacists in the interest of patient safety.
With knowledge of dosage forms, equivalencies, tapering tools, and the potential for compounding intermediate dosage forms when necessary, as well as the most frequent contact with shared patients, pharmacists can and should often play an active role in planning and providing feedback during and after benzodiazepine and z-drug tapers. Some pharmacists can assist in preparing tapering schedules.
Furthermore, collaborating and communicating with the pharmacist, especially when tapering is in progress, is beneficial, as the pharmacy maintains ongoing documentation on patient interactions and any issues/concerns they may have noted over time. Providing the pharmacy with a patient care plan for tapering will keep all healthcare providers informed, especially if the patient contacts the pharmacist if they are experiencing any withdrawal symptoms or are requesting early refills. Randomized controlled trials have shown sedative-hypnotics deprescribing rates of 43% when pharmacists and physicians worked in collaboration.1
Consider a tripartite agreement with the patient-pharmacist-physician. Having a patient use only one pharmacy for their prescriptions helps the pharmacist know and assess the patient and enables the physician to inform the pharmacist in advance of special requests.
Suggested Resources
Managing Benzodiazepine Use in Older Adults by the Centre for Effective Practice in Ontario is an excellent clinical tool which can be adapted for other ages.
Deprescribing Benzodiazepine Receptor Agonists: Evidence Based Clinical Practice Guideline issued by the College of Family Physicians of Canada is a helpful resource.
Prescribing Drugs of Dependence in General Practice Part B, by the Royal Australian College of General Practitioners includes a framework for accountable prescribing of benzodiazepines in a practical guide that physicians can use to minimize harm and maximize benefits to patients. There are terrific resources included such as examples of responses to patient requests for benzodiazepines, communications with patients, practice policies and forms, patient agreements, drug and alcohol assessment tool, and a GP Guide to Insomnia.
Canadian Guidelines on Benzodiazepine Receptor Agonist Use Disorder Among Older Adults has useful guidance on either preventing the development of Benzodiazepine use disorder or optimally assessing and treating older patients who have developed such a disorder. The tapering guidance is helpful and can be applicable for other ages.
Patient Pamphlet: Insomnia and Anxiety in Older People: Sleeping pills are usually not the best solution.
Toolkit: Less Sedatives for Your Older Relatives – A toolkit for reducing inappropriate use of benzodiazepines and sedative-hypnotics among older adults in hospitals.
Toolkit: Drowsy Without Feeling Lousy – A toolkit for reducing inappropriate use of benzodiazepines and sedative-hypnotics among older adults in primary care.
https://mysleepwell.ca/ has an online hub of cognitive behaviour therapy for insomnia.
Ementalhealth.ca has information for both patients and physicians.
Balancing the Risks and Benefits of Benzodiazepines – Jama Network
RxFiles patient handouts (SHIRP account required – free sign up for SK healthcare providers)
Acknowledgements
The College of Physicians and Surgeons of Saskatchewan gratefully acknowledges the College of Physicians and Surgeons of Manitoba for permitting its document, Prescribing Benzodiazepines & Z-Drugs, to be adapted in preparing this standard.
__________________________
1 Martin P, Tamblyn R, Benedetti A, Ahmed S, Tannenbaum C. Effect of a Pharmacist-Led Educational Intervention on Inappropriate Medication Prescriptions in Older Adults: The D-PRESCRIBE Randomized Clinical Trial. JAMA 2018:320:1889-98
|
STATUS:
|
APPROVED
|
|
Approved by Council:
|
November 2023
|
|
Amended:
|
n/a
|
|
To be reviewed:
|
November 2028
|